Mpox public health emergency declared over [1]
Tedros Adhanom Ghebreyesus was speaking to journalists in Geneva, a day after the emergency committee which made the emergency recommendation last July, advised the Director-General to declare it over.
‘Significant challenges’ remain
“However, as with COVID-19, that does not mean that the work is over. Mpox continues to pose significant public health challenges that need a robust, proactive and sustainable response”, cautioned Tedros.
He said there had been more than 87,000 cases, and 140 deaths worldwide reported to WHO, from 111 different countries.
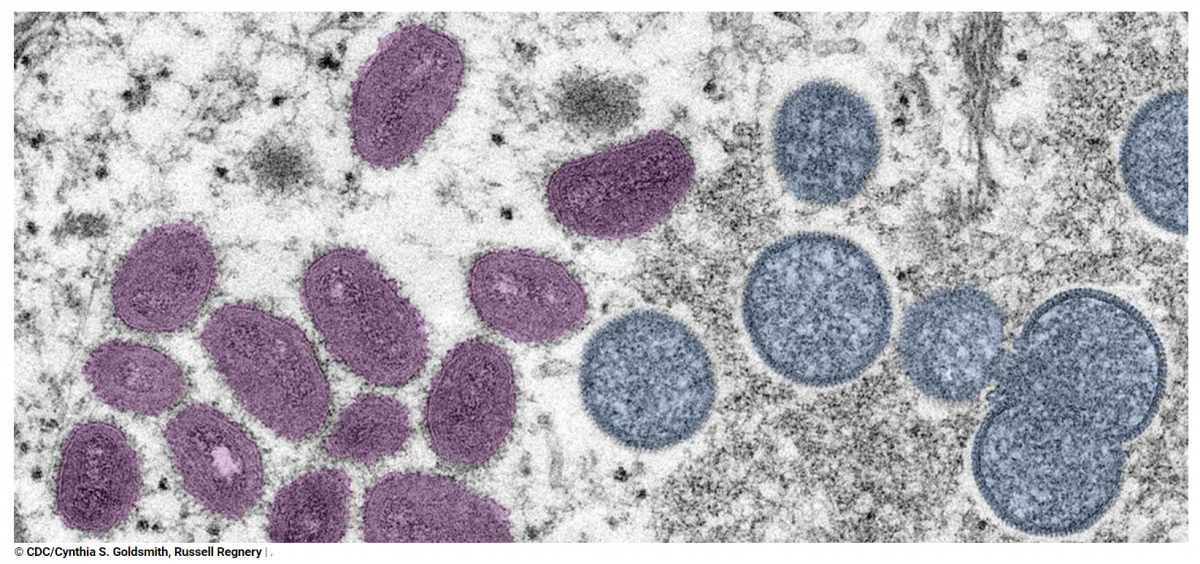
The virus, originally known as Monkey Pox, spreads through direct contact with bodily fluids and causes flu-like symptoms, and also pus-filled lesions on the skin.
Last July, it was spreading rapidly, but Tedros said WHO “has been very encouraged by the rapid response of countries. We now see steady progress in controlling the outbreak based on the lessons of HIV and working closely with the most affected communities.”
90 per cent drop in cases
Some 90 per cent fewer cases were reported in the past three months, compared with the previous three.
From the beginning of the international outbreak of the disease which has been in circulation since 1970, and occurred primarily in tropical rainforest areas of Central and West Africa, WHO stressed that most of those infected, recover without treatment in just a few weeks.
He praised the work of community groups, and public health authorities, saying their work had been “critical for informing people of the risks of mpox, encouraging and supporting behaviour change, and advocating for access to tests, vaccines and treatments to be accessible to those most in need.”
Cases of the virus were concentrated among men who have sex with men, especially those with multiple sexual partners.
Backlash avoided
Tedros noted that while stigma has been a driving concern in managing the mpox epidemic, and continues to hamper access to care, “the feared backlash against the most affected communities has largely not materialized. For that, we are thankful.”
He said despite the downward trend in cases, the virus was continuing to impact all regions, including Africa, where transmission “is still not well understood.”
There is a particular risk associated with those living with untreated HIV infections, he added, urging countries to keep testing capacity and be ready to respond promptly if cases rise again.
“Integration of mpox prevention and care into existing health programmes is recommended, to allow continued access to care, and rapid response to address future outbreaks.”
WHO will continue to work towards supporting access to countermeasures as more information on effectiveness of interventions becomes available.
Vice-Chair of the Emergency Committee, Professor Nicola Low, said there was a need to switch now from emergency measures, to managing the long-term public health risks of mpox, similar to national surveillance programmes that exist for infections such as HIV.
Watch for resurgence
“While the emergencies of mpox and COVID-19 are both over, the threat of resurgent waves remains for both”, said Tedros.
“Both viruses continue to circulate, and both continue to kill.
And while two public health emergencies have ended in the past week, every day WHO continues to respond to more than 50 emergencies globally.”
Health, front and centre
Tedros said that as the UN approached the upcoming World Health Assembly and three high-level meetings on pandemic preparedness, tuberculosis and universal health coverage, there were many challenges ahead, but also unprecedented opportunities.
If real commitments can be made, then real benefits could result, “for generations to come.”
Each meeting will be an opportunity to catalyse political commitment to drive progress, and to generate concrete action and financial resources, he continued.
“To invest in expanding access to prevention, testing, treatment, vaccines and research for TB; to strengthen the world’s defences against pandemics; and to strengthen health systems, especially primary healthcare, so that no one misses out on the care they need because of who they are, where they live or how much they earn.”